Why employers are realizing the need to follow compliance guidelines:
Organizations are facing more pressure than ever to strengthen their employee benefits packages to stay competitive in the marketplace, find top talent, and retain their best employees. But there’s more to consider than just offering a variety of benefits. When organizations fail to factor in compliance, the fines and penalties are steep.
Encouraging organizations to take it seriously isn’t a scare tactic or sales strategy. The penalties are real. The US Department of Labor reported that in FY 2022, the Employment Benefits Security Administration (EBSA) recovered $931 million in investigations. Of the 907 civil investigations, 66% resulted in financial results for plans or other corrective actions.
The bottom line is that if your organization hasn’t considered the compliance aspect of your employee benefits, now is the time.
First, let's cover the basics:
What is compliance?
Who has to follow compliance regulations?
Where do I start compliance planning?
What are the compliance requirements?
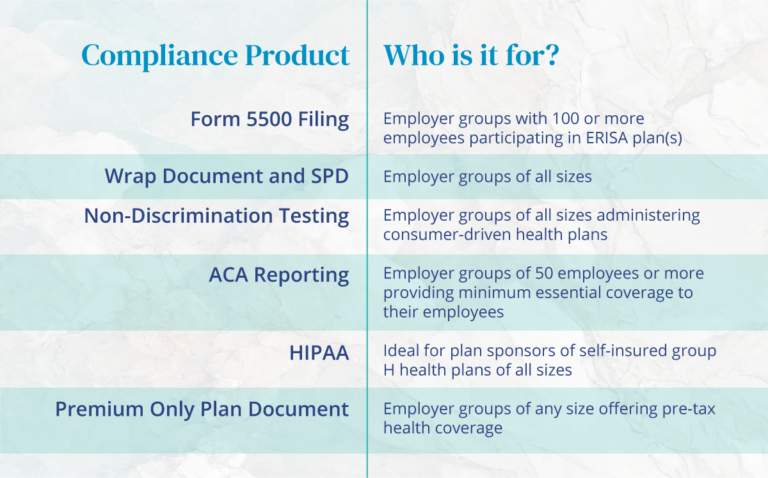
Planning, notification, documentation, and filing requirements may vary depending on your business size and the benefits offered. It’s crucial for the plan administrator to be aware of and follow these closely. It’s a long list, so to dig in deeper, here’s an overview:
As 2022’s high percentage of corrective actions indicates, organizations can handle it internally, but it can be overwhelming to maintain effectively.
For this reason, choosing a third-party-benefits administrator (TPA) benefits administrator like Ameriflex has its advantages:
- Mitigates the liability of having an internal administrator
- Helps to avoid conflicts of interest.
- Eliminates the overhead of an internal administrator and related office expenses
- Personalized customer service
- The expertise gained from years of experience
Ameriflex has been an industry leader for 20-plus years and provides expert compliance services and benefits administration. We will create a plan to best serve your employees and keep you on top of the requirements.